Diabetic Foot Problems: Symptoms, Treatment, and Care
Diabetes, a chronic health condition affecting millions worldwide, brings with it various complications, one of which is diabetic foot problems. These issues, if left unchecked, can lead to severe consequences. In this informative blog, we will explore the nature of diabetic foot problems, their symptoms, and effective treatment strategies. We'll also introduce the expertise of Dr. Ashutosh Shah and the Surat Diabetic Foot and Ulcers Clinic, renowned for their exceptional care in this field.
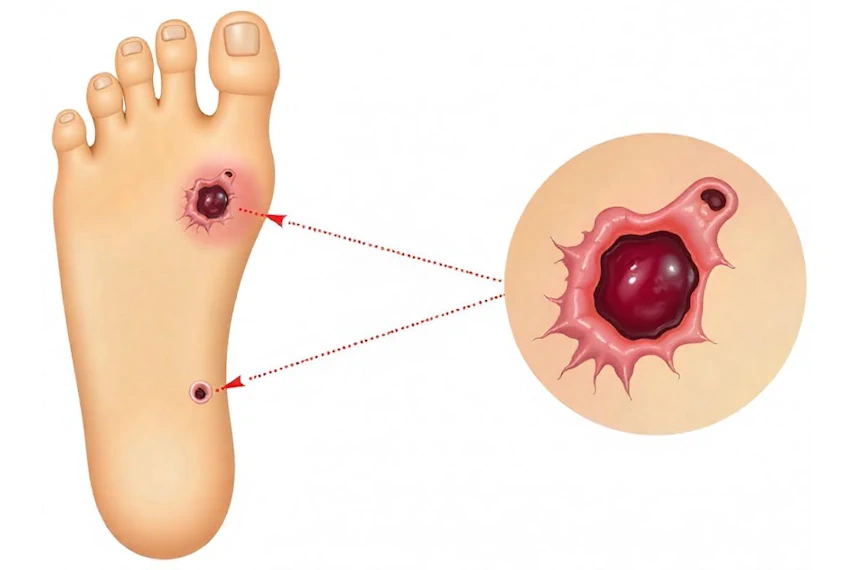
What is Diabetic Foot?
Diabetic foot is a term used to describe a range of foot problems commonly occurring in individuals with diabetes. Due to the high blood sugar levels associated with diabetes, nerve damage (neuropathy) and poor blood circulation are common, which can lead to foot complications. These problems can range from dry skin and calluses to more serious infections and ulcers. If not properly managed, diabetic foot issues can lead to severe consequences, including amputation in extreme cases.
Watch videos about Diabetic Foot:
Explore Videos related to Diabetic Foot
What are the Signs of Diabetic Feet?
Symptoms of diabetic foot problems can vary but often include numbness, tingling sensations, blisters or sores, changes in skin colour, and temperature variations in the foot. Early detection of these symptoms is key to preventing more serious complications. Recognising the signs of diabetic feet early is crucial for prevention and treatment. Common symptoms include:
- Numbness or a tingling sensation, indicating nerve damage.
- Swelling, redness, or warmth in the foot.
- Pain or discomfort in the legs.
- Dry skin, calluses, or cracks in the feet.
- Change in the colour and temperature of the feet.
- Slow-healing sores or ulcers on the feet.
- Foul-smelling discharge from a foot wound.
- Causes of Diabetic Foot?
The primary causes include:
Neuropathy: High blood sugar levels can cause nerve damage, leading to loss of sensation in the feet.
Poor Circulation: Diabetes can affect blood flow, making it harder for a foot injury or infection to heal.
Immune System Deficiency: Diabetes can weaken the immune system, reducing the body's ability to fight off infections.
Foot Deformities: Diabetes can cause changes in the feet, like hammertoes or bunions, which can create pressure points and lead to ulcers.
What are the 5 Stages of Diabetic Foot?
Stage 1: Initially, there may be minor skin changes without ulceration. The feet may be dry with cracked skin.
Stage 2: Development of ulcers without infection. These are typically superficial and can be treated with proper wound care.
Stage 3: Ulcers become infected. The infection may be localized to the ulcer site or may start affecting deeper tissues.
Stage 4: The infection progresses, leading to localized gangrene. The affected area may become black due to lack of blood flow.
Stage 5: Extensive gangrene that may require amputation. This is the most severe stage and indicates a critical need for medical intervention.
How Does Diabetic Foot Start?
It often starts with minor injuries or changes in the skin, such as blisters, cuts, or calluses. Due to reduced sensation from neuropathy, these injuries might not be felt and can worsen without proper care. Poor blood circulation also means these wounds heal slowly, increasing the risk of infection and complications.
Who is at Risk for Diabetic Foot Conditions?
Individuals with poorly controlled diabetes, a long history of diabetes, or those with other health issues like obesity or heart disease are at higher risk. Regular check-ups and proper diabetes management are crucial for these individuals. Individuals most at risk include:
- Those with poorly controlled diabetes.
- Long-term diabetics.
- People with diabetic neuropathy or circulation problems.
- Diabetics who use insulin.
- Smokers.
- Those with a history of foot ulcers or amputations.
By understanding these aspects of diabetic foot care, individuals can take proactive steps to prevent complications and maintain healthy feet. Regular consultations with healthcare professionals like Dr. Ashutosh Shah and his team at the Surat Diabetic Foot and Ulcers Clinic can provide personalized care and treatment plans.
Conclusion:
Diabetic foot problems, while serious, can be effectively managed and prevented with proper care and early intervention. Understanding the signs, risk factors, and treatment options is crucial for individuals with diabetes. Regular check-ups and expert guidance, like that provided by Dr. Ashutosh Shah and his team, play a vital role in maintaining foot health in diabetic patients.
For expert care and consultation on diabetic foot problems, contact the Surat Diabetic Foot and Ulcers Clinic. Led by the experienced Dr. Ashutosh Shah, the clinic offers a range of treatments and preventive care options. Visit Surat Diabetic Foot and Ulcers Clinic or call +91 8849066499 for more information.
FAQs
How often should someone with diabetes check their feet?
A: Daily foot checks are recommended to catch any cuts, blisters, or changes early.
What are the best ways to prevent diabetic foot problems?
Maintaining good blood sugar levels, regular foot inspections, wearing appropriate footwear, and avoiding walking barefoot can help prevent problems.
Can diabetic foot ulcers be completely healed?
Yes, with proper treatment, diabetic foot ulcers can be healed. Early intervention and consistent care are crucial. .
How can I tell if I have nerve damage in my feet?
Signs of nerve damage include numbness, tingling, burning, or a loss of sensation in the feet. Regular check-ups with a healthcare provider are important for detection and management .



.jpg)

